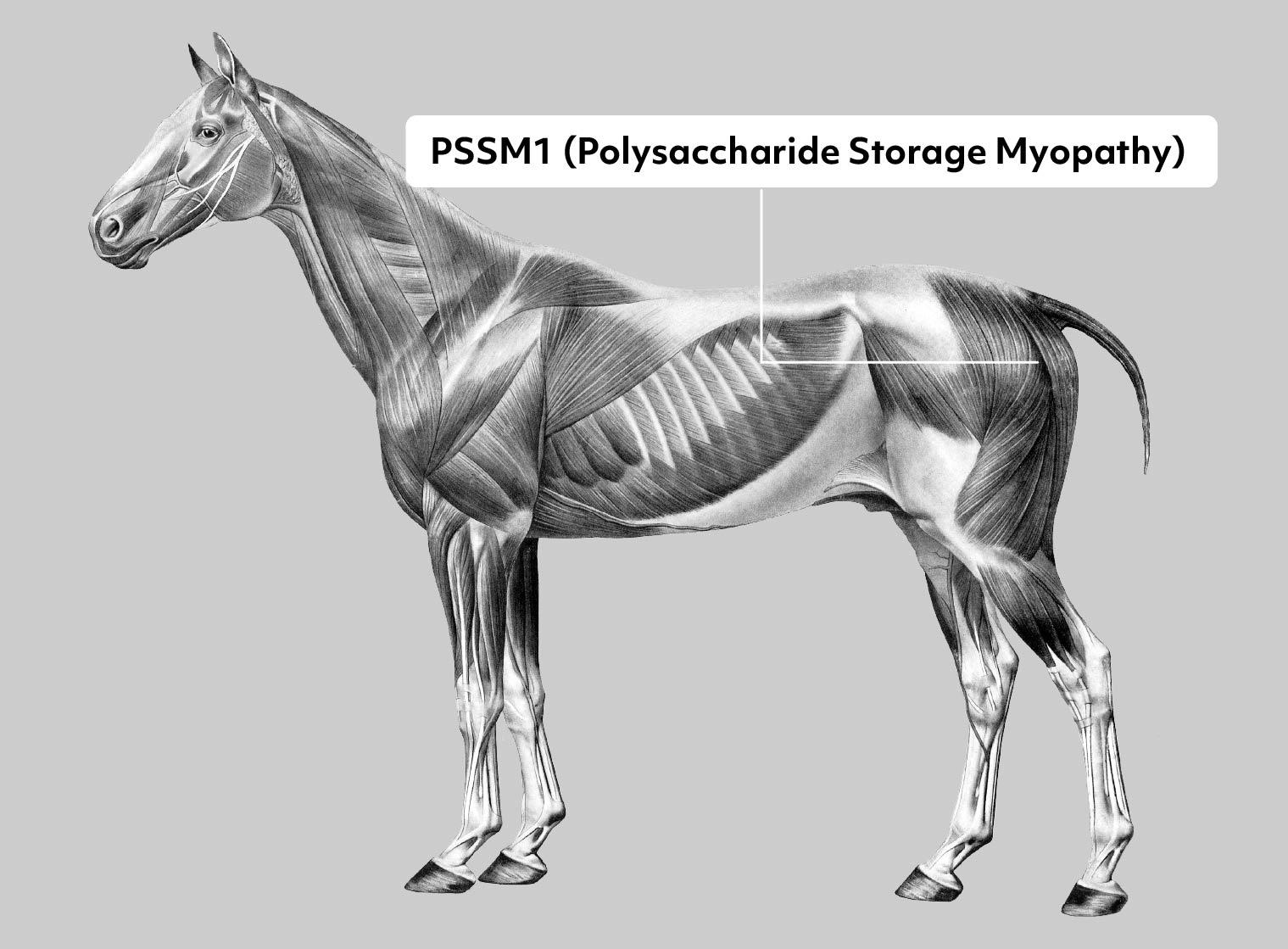
Polysaccharide Storage Myopathy (PSSM1)
Gene or Region: GYS1
Reference Variant: C
Mutant Variant: T
Affected Breeds: Many
Research Confidence: High confidence - Findings reproduced multiple studies
Explanation of Results: PSSM1/PSSM1 = homozygous for Polysaccharide Storage Myopathy, extreme trait expressed PSSM1/n = heterozygous for Polysaccharide Storage Myopathy, trait expressed n/n = no variant detected
General Information for Polysaccharide Storage Myopathy (PSSM1)
Polysaccharide Storage Myopathy (PSSM) is a glycogen storage disorder in which affected horses have chronic episodes of exertional rhabdomyolysis (“tying-up”). Acute symptoms are an unwillingness to move and muscle damage following exercise. Heterozygous horses (PSSM1/n) experience more moderate symptoms that can usually be managed through a low-sugar/starch diet and exercise. However, homozygous horses (PSSM1/PSSM1) are generally more severely affected and are thus harder to manage. Additionally, one study has found that horses with PSSM1 and a malignant hyperthermia (MH) exhibit more severe clinical symptoms.
GYS1 is an enzyme involved in the production of glycogen that is found specifically within the muscle. Mutations in this gene have been associated with glycogen storage diseases in several species. This particular mutation is a single base substitution that alters an amino acid, likely affected the function of the encoded protein.
References
McCue ME et al., “Glycogen synthase (GYS1) mutation causes a novel skeletal muscle glycogenosis.” (2008) Genomics. 91: 458-66. PMID: 18358695
McCue ME et al., “Glycogen synthase 1 (GYS1) mutation in diverse breeds with polysaccharide storage myopathy.” (2008) J Vet Intern Med. 22: 1228-33. PMID: 18691366
Herszberg B et al., “A GYS1 gene mutation is highly associated with polysaccharide storage myopathy in Cob Normand draught horses.” (2009) Anim Genet. 40: 94-6. PMID: 18822097
McCue ME et al., “Polysaccharide storage myopathy phenotype in quarter horse-related breeds is modified by the presence of an RYR1 mutation.” (2009) Neuromuscul Disord. 19: 37-43. PMID: 19056269
Tryon RC et al., “Evaluation of allele frequencies of inherited disease genes in subgroups of American Quarter Horses.” (2009) J Am Vet Med Assoc. 234: 120-5. PMID: 19119976
Stanley RL et al., “A glycogen synthase 1 mutation associated with equine polysaccharide storage myopathy and exertional rhabdomyolysis occurs in a variety of UK breeds.” (2009) Equine Vet J. 41: 597-601. PMID: 19803057
Baird JD et al., “Presence of the glycogen synthase 1 (GYS1) mutation causing type 1 polysaccharide storage myopathy in continental European draught horse breeds.” (2010) Vet Rec. 167: 781-4. PMID: 21262610
McCoy AM et al., “Evidence of positive selection for a glycogen synthase (GYS1) mutation in domestic horse populations.” (2014) J Hered. 105: 163-72. PMID: 24215078
More Horse Health
Equine Herpes Virus Type 1 & Induced Myeloencephalopathy
Equine herpesviruses are DNA viruses that are found in most horses all over the world, often without any serious side effects. Following infection of Equine Herpesvirus Type 1 (EHV-1) some horses then suffer Equine Herpesvirus Myeloencephalopathy (EHM), which is is accompanied by serious and sometimes fatal neurological effects. EHM in horses can have serious neurological symptoms on affected horses.
Equine Metabolic Syndrome / Laminitis Risk
Equine Metabolic Syndrome (EMS) is a wide-spread issue in the horse population. Primarily characterized by hyperinsulinemia (excess insulin circulating in the blood in relation to glucose levels), this metabolic disorder is often present in obese horses and ponies and can be challenging to diagnose as it can be misdiagnosed as "Cushing's" (a pituitary disfunction).
Equine Recurrent Uveitis Risk and Severity
Equine Recurrent Uveitis (ERU) is the most common cause of blindness in horses, affecting about 3-15% of the horse population worldwide. Characterized by episodes of inflammation of the middle layer of the eye, Equine Recurrent Uveitis in horses leads to the development of cataracts, glaucoma and eventually complete loss of vision.